手部瘢痕挛缩是一种常见的临床问题,其特征是关节活动度受限。与关节本身挛缩不同,这类挛缩通常发生在肢体末端,尤其是关节处,且与长期存在的线性瘢痕有关。本期我们带来日本医科医院整形、重建与美容外科Dr. Hoyu Cho《Management of Scar Contractures of the Hand—Our Therapeutic Strategy and Challenges》,介绍手部瘢痕挛缩的处理。

图1:Cause of contracture. Contractures can be broadly classified into cases where the cause is outside the joint (extra-articular element) and cases where the cause is within the joint itself (intra-articular element). Scar contracture is caused by an extra-articular element, the skin
分型和一般处理
根据瘢痕挛缩的具体特征,如其位置、形状和大小,将其分为4型:1型(浅线性)、2-d型(深线性)、2-s型(局限于浅层的平面瘢痕挛缩)和3型(到达深层的平面瘢痕挛缩,即三维瘢痕挛缩)。

图2:Dimensional classification of scar contracture. Scar contractures are morphologically divided into superficial and deep, linear and planar, and are classified as follows: Type 1 (superficial linear scar contracture), Type 2-d (deep linear scar contracture), Type 2-s (planar scar contracture confined to the superficial layer), and Type 3 (planar or three-dimensional scar contracture reaching deep layers)
1型通常由轻微割伤引起,2-s型由二度烧伤引起,2-d型由关节附近手术引起,3型由严重创伤如压伤引起。3型除了瘢痕挛缩外,还可能并发关节挛缩。
确定手术方式三因素:缺损的大小、缺损周围健康皮肤的可用性以及缺损床的血液循环。
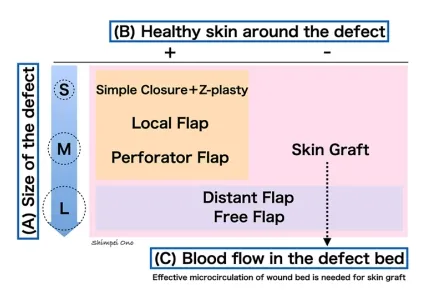
图3:A treatment strategy for hand scar contracture. To decide on the treatment strategy for defects after releasing the scar contracture, there are three judging points: (A) the size of the defect, (B) the presence of healthy donor skin around the defect, and (C) the condition of the vascular bed.
S, Small-size; M, Medium-size; L, Large-size
1型和2-d型为线形疤痕:切除瘢痕并以直线缝合,使用z-成形术或其改良方法释放挛缩。
2-s型,瘢痕挛缩带解除后,小缺损采用局部皮瓣,中等缺损采用带蒂穿支皮瓣,大缺损采用游离皮瓣和远端皮瓣。2-s型在缺陷床有良好的血液循环,所以无论缺陷大小,全层皮肤移植也是一种合适的选择。
3型,释放深层瘢痕挛缩会暴露出血液循环不良的重要结构,如肌腱、关节和骨骼。因此,建议采用皮瓣而非皮肤移植的手术方案。
手术
手术指征:需要改善功能和美观的严重病例、要求提高美观度的轻微功能损害病例。
手术时机:一般瘢痕成熟后手术,但严重功能受限的挛缩,有发展为关节挛缩的趋势,应立即进行手术。儿童PIP关节长期固定在屈曲位置,会损害指的伸展机制,因此一旦伤口愈合并发生挛缩,需要早期手术干预。
手术策略:在手部瘢痕挛缩的治疗中,使用局部健康皮肤、局部皮瓣或带蒂穿支皮瓣进行皮瓣重建通常比皮肤移植更可取。
为了避免植皮后的二次挛缩,通常推荐全层植皮治疗瘢痕挛缩。
选择皮瓣,在捆绑固定期间不需要休息,术后早期即可以开始康复。
如果瘢痕挛缩周围有足够健康的皮肤,尽可能多地切除疤痕。反之,如果瘢痕挛缩处周围没有足够健康的皮肤,则不宜强行切除瘢痕。瘢痕挛缩线沿纵向在挛缩最强烈的部位划分。
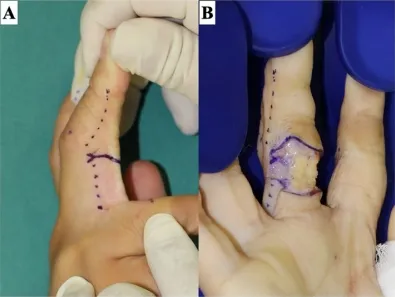
图4:Release of a scar contracture line on a finger. Releasing the scar contracture line causes a skin defect. The stronger the scar contracture, the larger the defect size. The skin incision is made slightly beyond the midlateral line (dotted line), and the Y-shaped incision creates a zig-zag wound edge to prevent re-contracture. The scar tissue in the defect bed is sufficiently dissected and excised until healthy fat tissue is identified. (A) The design of the skin incision line. (B) After releasing the scar contracture line
特别是在解除指掌挛缩时,为防止复发,皮肤移植或皮瓣的背侧边缘应在背侧方向与中外侧线重合或延伸至中外侧线以外。
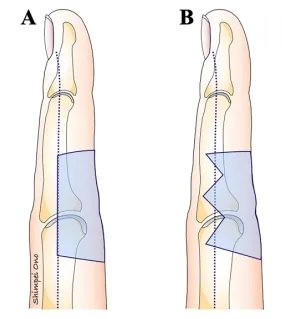
图5:The shape of the defect after the release of a scar contracture on the palm side of the digit.
If the defect edge matches the midlateral line or crosses it to the dorsal side, it will be difficult for thegrafted skin to undergo secondary contraction. (A) The dorsal edge of the donor aligns with the midlateral line of the digit.(B) The dorsal edge of the defect extends the midlateral line of the digit with a zig-zag shape.
垂直于指掌侧皮肤皱褶的纵向缝合线可引起增生性疤痕和瘢痕挛缩复发。因此,可以通过定位皮肤使缝合线在该区域形成之字形或在缝合线穿过皮肤折痕处添加一个小的z形成形术来防止瘢痕挛缩。

图6:The design of a z-plasty for a linear scar that is perpendicular across the creases of the digit.
(A) A scar that is perpendicular to the digital crease tends to cause scar contracture. Therefore, the z-plasty needs to be oriented on the crease. (B) The z-plasty is designed so that the lateral limbs match the digital crease after the flap is transposed
要确保导致瘢痕挛缩的纤维组织完全切除。如果引起挛缩的疤痕组织没有完全切除,手术的侵入性可能会加剧疤痕挛缩。
术后管理
瘢痕挛缩术后仍需进行固定、康复等措施,以防出现再次挛缩。
瘢痕挛缩解除后,目标关节应固定。通常使用外固定。手术后2至3周内除康复训练时间外,均应固定。此后可以仅夜间固定,持续至少三个月。当发现哪怕是最轻微的疤痕硬化时,也应立即开始夜间使用类固醇胶布。
术后应立即将肢体冷却并抬高,并保持抬高1-2周。
伤口愈合后(通常在术后一至两周),应开始目标关节的康复,温和主动活动可以促进淋巴和静脉回流,防止手部水肿。关节的主动和被动活动应经常进行(每小时约5分钟),而不引起患者疼痛。
儿童病例推荐克氏针临时固定以保持正确的位置。克氏针的插入时间应尽量短,避免关节挛缩,术后1-2周内取出克氏针。